While death is a natural part of life, many people find it hard to bring up end-of-life discussions with their loved ones and even their doctors. More than 90 percent of people think these conversations are important, yet fewer than 30 percent have actually had them with their families.
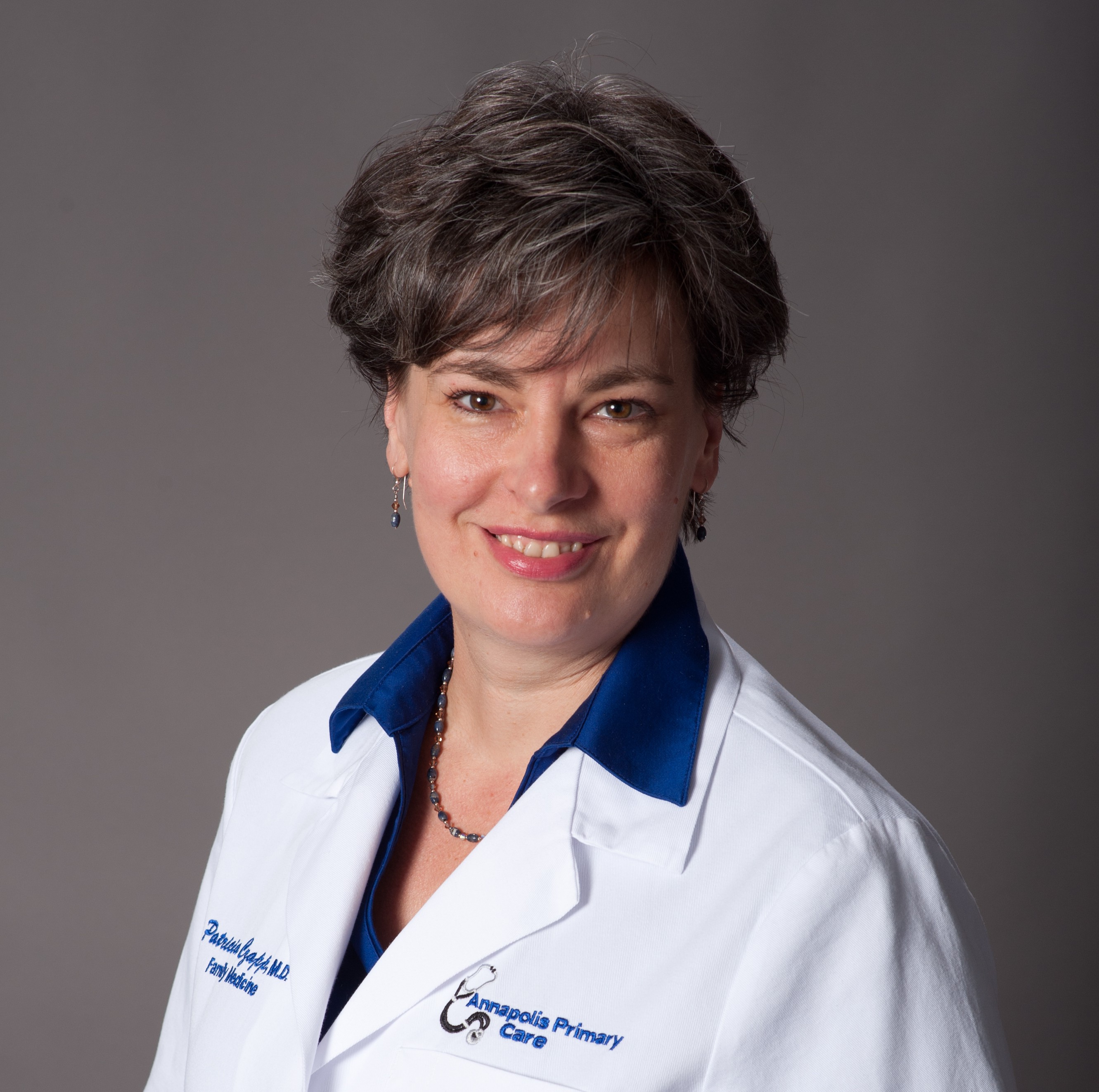
It may seem impossible to plan for the end of life, but Patricia Czapp, MD, chair of clinical integration at Anne Arundel Medical Center, explains death isn’t a surprise for most people. “You need a general plan,” she says. “It should involve really good conversations about what’s important to you in your life and, more importantly, who will make decisions for you if you can’t speak for yourself.”
Dr. Czapp says your spokesperson should be someone you trust, whether that’s a relative or close friend. It’s important to identify someone and have a conversation about your wishes, even though bringing it up can be uncomfortable.
AAMC is proud to partner with The Conversation Project, a group that recognizes the difficulty and importance of these conversations. The Conversation Project offers resources like the Conversation Starter Kit that breaks down the discussion process into four easy steps: get ready, get set, go and keep going.
“They guide you through the things you should be thinking about: What level of quality of life would you like? Are you willing to go to a nursing home if you might never come home? What would it be like if you couldn’t talk or you couldn’t recognize your family members anymore?,” says Dr. Czapp. “Those are things you’ve got to have a conversation about. If you wait until it’s too late and you’re in the emergency room it doesn’t always go very well. You don’t have time to process it all.”
READ MORE: The Conversation Project: Sharing your wishes for end-of-life care
Advance directives are also important. They are written instructions that explain your healthcare decisions if you are no longer able to speak for yourself. However, the decisions you make when preparing the advance directive may be different than the ones you would make when you become ill.
This is why Dr. Czapp recommends having a spokesperson to make decisions for you. A spokesperson can talk to your doctor and help apply the decisions you made in your advance directive to your current health status.
Just as you have end-of-life conversations with your loved ones, you should also have them with your doctor. It is important that your doctor understands your wishes and beliefs in order to help you. Medicare now pays for these face-to-face meetings about end-of-life care.
“Eventually, everybody’s life comes to an end and if we can stop denying that then we can say, ‘How do I plan for the best ending?’” concludes Dr. Czapp.
What is palliative care?
Here are the top three things you need to know about palliative care from Dr. Czapp:
- Palliative medicine focuses on quality of life, symptom management, care planning and skillful decision-making that involve the body, mind and spirit.
- Palliative care is reserved for people who have a serious illness that can be life-threatening.
- Palliative care and hospice care share a similar whole-person, comprehensive approach. However, hospice is reserved for people who have a short life expectancy.
Contributor
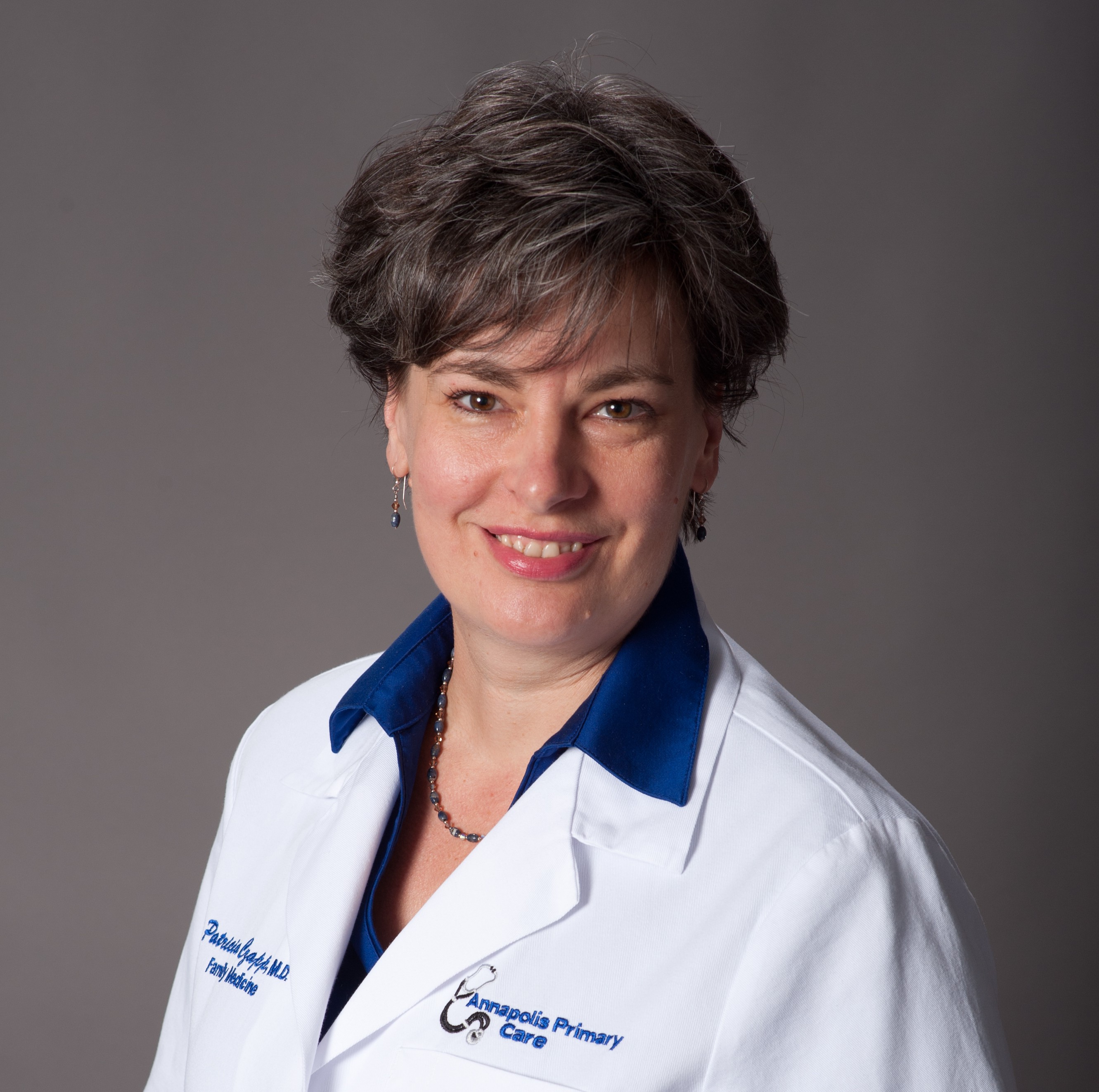 Patrica Czapp, MD
Patrica Czapp, MD, is the chair of clinical integration at Anne Arundel Medical Center.
Originally published Dec. 23, 2015. Last updated June 7, 2018.